by Dr. Adkins | Apr 2, 2021 | Blog, Dental Topics 1, Oral Surgery
Wisdom teeth are the third set of molars, and usually emerge in the late teens or early twenties. Standard dental practice is to remove wisdom teeth prior to them being fully formed when the roots have not yet had a chance to develop and fully root into the jaw. Younger patients usually have an easier recovery from surgery and many dentists believe early removal prevents future dental problems associated with wisdom teeth.
If your wisdom teeth were not removed as they emerged, there are some signs and symptoms that would indicate the need for extraction including:
- Wisdom teeth that are impacted, which means they have become trapped in the jawbone or gums.
- Wisdom teeth that are emerging at an awkward angle, causing pressure on adjacent teeth.
- Wisdom teeth that do not fit in your mouth, causing crowding of the surrounding teeth as well.
- Wisdom teeth that are suffering from decay or disease caused by the inability to keep them cleaned properly.
- Wisdom teeth that have developed fluid-filled cysts near the gumline.
- Wisdom teeth that are causing pain due to any of the above reasons.
The decision about whether or not to remove your wisdom teeth should be made in consultation with your dental professional. Your dentist or oral surgeon can assess the position and health of your wisdom teeth and make a recommendation for treatment.
If extraction is recommended, they may choose to extract one tooth or all four molars at once. Recovery from the outpatient procedure takes just a few days, and you will quickly be back to normal. Contact our dental office if you are experiencing any of these symptoms listed to determine if you should consider wisdom tooth removal to ensure your future good oral health.

by Dr. Adkins | Dec 25, 2020 | Blog, Dental Topics 2, Oral Surgery
While minor gum recession can be treated by your dentist with deep cleaning and antibiotics, serious gum recession can only be treated with oral surgery. A loss of bone and gum pockets that are very deep require gum surgery to address the pain and damage left by acute gum recession.
Three treatments are used primarily in the treatment of serious gum recession, in order of invasiveness: pocket depth reduction, regeneration, and soft tissue graft. Pocket depth reduction involves a deep cleaning of the affected area. The periodontist folds the gum tissue back and utilizes tooth scaling and root planing to remove any tartar and plaque built up around the tooth. Once the gum pockets are clean, the surgeon pulls the gum tissue gently around the tooth, eliminating the deep pockets altogether or significantly reducing their depth.
Regeneration utilizes a similar treatment to pocket depth reduction, but it also addresses any bone loss that occurred due to acute gum recession. In this process, a regenerative agent such as graft tissue, membranes or tissue stimulating proteins is added to the affected area. The gum tissue is then tucked into place and stitched down. Over time, the regenerative agent will work to rebuild lost bone and tissue, leaving healthy and thriving tissue behind.
The most common soft tissue graft is taken from the patient’s own mouth, either by removing tissue from the roof of the mouth or from the gum tissue near the affected tooth. The healthy gum tissue is placed in the affected area, over the exposed tooth root, protecting it from infection and damage.
To prevent the need for oral surgery to address your receding gums, have good oral hygiene habits. Brush, floss and see your dentist twice a year for checkups and professional cleanings. Talk to your dentist if you have any other questions about how to reverse or prevent gum recession.
We treat patients from McDonough and the surrounding area
by Dr. Adkins | Dec 18, 2020 | Blog, Dental Topics 1, Oral Surgery
Wisdom teeth, your third set of molars, are named that because they are the final teeth to erupt. They usually come in between ages 17 to 25, and are located in the very back of your mouth on the top and bottom. Your dentist will examine you to find out if your wisdom teeth are properly positioned and healthy. If they aren’t, your dentist will recommend removal.
How do you know wisdom teeth should be removed?
Some of the signs there is a problem with your wisdom teeth include pain, infection, cysts, gum disease, damage to nearby teeth, and tooth decay. If you experience any of these symptoms, see your dentist for an examination.
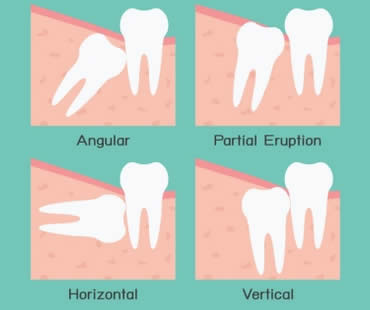
What are impacted wisdom teeth?
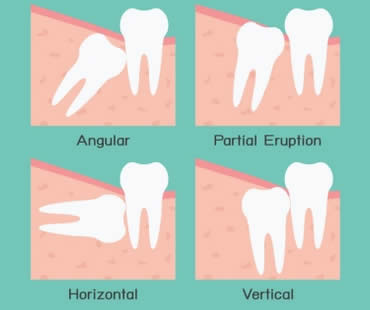
Sometimes your teeth just don’t have room to grow in properly. They can erupt at angles within your jaw, sometimes even horizontally. If wisdom teeth aren’t able to erupt normally they can become trapped, or impacted, inside your jaw. Symptoms of impacted wisdom teeth are pain, infection, and swelling. When teeth are impacted, they can lead to serious problems. Many dentists want to avoid impacted teeth and therefore remove your wisdom teeth before they erupt or grow too big.
Are there less obvious reasons to remove wisdom teeth?
It’s not always clear when these teeth way in the back of your mouth are causing problems, or might in the future. Many dentists remove them in teens or young adults so they don’t cause problems later, or become too firmly planted in the jaw. Also, sometimes wisdom teeth are removed as part of orthodontic, periodontal, or restorative treatment plans.
What happens if I don’t have them removed?
Some dentists prefer to wait and see what happens with time to your wisdom teeth. Make sure you continue to have these teeth monitored, because the risk of problems doesn’t go away with age. Removing wisdom teeth isn’t always necessary, because if there’s room in your mouth and they come in properly, they work just like any other teeth. The key is to watch them to make sure problems don’t arise in the future.
Dental office for wisdom teeth removal

by Dr. Adkins | Oct 23, 2020 | Blog, Dental Topics 2, Oral Surgery
There are a number of reasons that dentists or oral surgeons recommend surgery, but facial injuries are probably the most unexpected and alarming cause. Maxillofacial injury, or facial trauma, refers to any injury to the mouth, jaw, and face. Most of these injuries result from sports, car accidents, job accidents, violence, or an accident at home. Let’s learn about oral surgery resulting from facial trauma.
Broken bones are a common type of serious facial injury. Fractures can occur in the upper or lower jaw, cheekbones, palate, and eye sockets. Injuries in these locations may affect vision and the ability to eat, talk, and breathe. Hospitalization is often required for treatment, which is similar to that for fractures in other parts of the body. The bones must be lined up and held in place to allow time to heal them in the correct position. Because casts are not possible in facial injuries, the surgeon may use wires, screws, or plates to treat fractures. Sometimes healing takes as long as six weeks or more.
Even though some facial injuries are worse than others, all of them should be taken seriously. They affect an important area of the body, so it is recommended to seek treatment from an oral surgeon to make sure you receive optimum care. Even if stitches are all that’s required, it’s best to have them performed by an oral surgeon who can place them exactly as needed to produce the best results.
It’s no surprise that the best solution for facial injuries is to prevent them in the first place. Oral surgeons suggest consistent use of mouth guards, seat belts, and masks and helmets as required. Improvements have been made to safety gear to make these items more comfortable and efficient, so there should be no excuses for not using them to protect yourself and avoid injuries that can lead to oral surgery.
If you need a dentist in McDonough contact us today

by Dr. Adkins | Feb 21, 2020 | Blog, Dental Topics 2, Oral Surgery
Obstructive sleep apnea is a condition created when a portion of the upper airway is blocked, causing breathing interruptions during sleep and low blood oxygen levels. As many as 20% of adults are affected by mild obstructive sleep apnea, while one in fifteen suffers from more severe apnea.
Symptoms of obstructive sleep apnea include snoring, extreme daytime drowsiness, restless sleep, high blood pressure, depression, problems with mental function, as well as a host of other mental and physical concerns. Left untreated, obstructive sleep apnea can lead to a long list of serious medical conditions, including hypertension, heart attack and stroke.
If you have been diagnosed with obstructive sleep apnea, your doctor may initially treat the condition with a CPAP device that you wear while sleeping. While a CPAP machine will reduce the obstruction to the airway, it is not a cure and will only be effective during use. Other non-surgical treatment recommendations may include the wearing of mouthguards to reposition the jaw, sleep position changes, or weight loss.
Tongue muscle advancement involves moving the bony attachment of the tongue muscles, and can be combined with palatal surgery to reduce excess tissues. This therapy may also include removing enlarged tonsils and nasal surgery. These treatments are most often used for milder cases of obstructive sleep apnea.
However, if these treatments do not work or for more severe cases of obstructive sleep apnea, oral surgery offers solutions to correct apnea. Maxillomandibular Advancement is a procedure that repositions the upper and lower jaw and chin to open the airway. This treatment is highly successful and offers the greatest chance of permanent correction in moderate to severe cases of obstructive sleep apnea.
For more information about how surgical therapies and treatments can be utilized to address your obstructive sleep apnea, consult with a qualified oral and maxillofacial surgeon.
Our dental office is located in McDonough

by Dr. Adkins | Feb 7, 2020 | Blog, Dental Topics 2, Oral Surgery
If oral surgery is in your future, you might be worried about what’s to come. The way to relieve that worry is to talk to your oral surgeon. Your oral surgeon has the experience and knowledge necessary to guide you through whatever concerns or questions you may have. Here is a guide to some of those questions and answers:
How will I handle pain following surgery?
- In many cases, you will have been prescribed narcotic pain relievers. If you are taking narcotics, take them only as recommended and do not mix them with over-the-counter pain relievers or alcohol. Driving while on narcotics is dangerous and can have serious consequences for you personally and for others. If you weren’t prescribed any medication, use anti-inflammatory analgesics such as ibuprofen or naproxen sodium.
What will happen to my stitches in the days following surgery?
- Some stitches will be designed to dissolve over time and will not need to be removed. Others will not come out on their own and will need to be removed at a subsequent appointment. In many cases, losing a single stitch or two in the days following surgery isn’t serious; however, for bone-graft treatments, it is problematic and you should contact your surgeon immediately.
Can I eat normally after surgery?
- Immediately after surgery when you’re still experiencing any mouth or tongue numbness, don’t eat anything. You could mistake the soft tissues of your mouth for food and do serious damage to your mouth without realizing it. After your numbness subsides, consume soft foods of tepid temperatures for several days to allow for healing. Talk to your surgeon to learn when you can resume normal eating patterns as dictated by your particular surgery.
What other tips do you have?
- Stay hydrated and rest as much as possible to facilitate complete and quick healing. Call your surgeon if you have excessive bleeding or pain that doesn’t lessen with time. Be aware of signs of infection (swelling, redness, odorous or sour discharge) at the surgical site and seek professional care when needed.
If you need a dentist in McDonough contact us today





 (470) 665-5292
(470) 665-5292  E-Mail Us
E-Mail Us 
